












Win a free bottle of Uribiotic
Your feedback is important to us.
Please tell us what you like most about any of our UTI Products from your own experiences using them.
At the beginning of every month we will pick our favourite entry as the winner and publish it on this site.
In appreciation for your time, you will receive a free bottle of Uribiotic.
Click here for details
|
|
|
UTI Signs Symptoms |
UTI Causes Risk Factors |
UTI E. Coli |
UTI Antibiotics |
UTI Catheters |
UTI Health Tips |
Uribiotic Testimonials
Urinary Tract Infection Remedy
Safe and Effective Lifeline for Those in Need for Natural Help
What All Conscious Women Must Know
From time to time, you may hear or read scientific reports allegedly showing that such-and-such vitamin doesn't work or may even be harmful to your health.
They are a perfect example of the existing, and often uninformed, prejudice against nutritional supplements.
I sincerely hope that you do not believe in such anti-vitamin nonsense discouraging their use; and - most importantly - you won't allow these saboteurs distract you from achieving and maintaining your health through the natural means.
|
Bladder infection or urinary tract infection (UTI), especially in adult females, has become a major medical problem.
Affecting over 13 million people each year in the United States, it is the most common infection in adult females (30:1 female:male ratio). In fact, it is a worldwide health problem.
This website is intended to allow you - a bladder infection sufferer - to become an informed patient who can manage her own care, ask the right questions, insist on adequate management and information, and seek an optimal outcome for yourself.
Perhaps it will even help health professionals who are giving care - urologists, gynecologists, obstetricians - to appreciate and, hopefully, consider the alternative UTI treatment, more natural and lifestyle-based.
When it comes to bladder care, you need to stay alert, ask questions, and ultimately rely on yourself for important healthcare decisions. By applying these guidelines, you will be able to take control of your health, just as we all should do.
Up to 60 percent (6 women in 10) of all women have at least one distinctly painful bladder infection during their lifetimes. Unfortunately, nearly 20 percent of women who have a bladder infection will have another, and 30 percent of that group will have yet another bout.
Of the last group of women, 80 percent will have bladder infection recurrences - with recurrences being most common in the age groups 25-29 and over 55 years.
For example, in the United Kingdom alone, it is estimated that one woman in three will have a UTI before the age of 24, and that half of all women will have at least one UTI during their lifetime. It is a worldwide problem, says professor Chris Thomas, an expert in bacteria at the University of Birmingham.
|
|
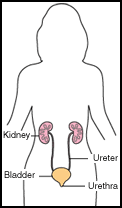
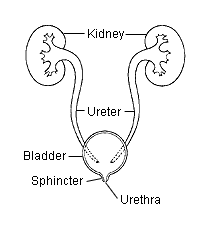
There are many types of urinary tract infection depending on the
part affected:
- the kidneys
- the ureters
- the bladder
- the urethra.
These organs produce, store, and eliminate urine - a combination of water and waste products that passes out of the body as fluid.
Despite its unsanitary image, the urine inside the bladder is normally sterile, free of bacteria. In fact, it has been called the "last clean stream in America!"
| |
Urine contains large quantities of urea - the colorless, crystalline end product manufactured within the liver - which is excreted from the body via urinary tract.
Known for its antiseptic and bactericidal properties, urea helps to inhibit the growth of many types of detrimental bacteria including:
- E. coli bacteria (uropathogenic Escherichia coli/UPEC) and
- Staphylococcus aureus (gram-positive aerobe, responsible for "Golden Staph").
It is also present in the skin where it functions as one of the endogenous components of the skin's natural moisturizing factor.
However, the vaginal area has bacteria that live in this warm, moist environment. These bacteria can start to move up the urethra and, if they reach the bladder, begin to multiply.
Normally, vaginal bacteria are flushed out of the urethra by urination before this can happen. Sometimes, however, for a variety of reasons, the bacteria take hold and cause an infection.
UTI in Women: Development of Symptoms
The farther into the urinary tract the infection progresses, the greater the number of symptoms.
|
Urinary tract infection (UTI) symptoms tend to be cumulative as the infection becomes more severe.
Although not everyone with a urinary tract infection has symptoms, most people get at least some, such as
- a frequent urge to urinate - having to go a lot, feeling that you have to urinate immediately during the day and/or night (sometimes incontinence may occur), and
- a sharp pain or painful, burning sensation with itching in the area of the bladder or urethra during urination (dysuria).
Symptoms of bladder infection can develop:
- quite rapidly - over a matter of hours, or
- more slowly - nagging for several weeks.
Mild cases of acute urinary tract infeciton may disappear spontaneously without any treatment.
UTI in Women: Urethritis
This is a bacterial infection or inflammation of the urethra (tube that carries urine from the bladder) which is more frequent in men than in women; it often sets the stage for the development of cystitis.
UTI in Women: Cystitis
This is a bacterial infection or inflammation of the urinary bladder. It is the most common infection - 50 times more common in women and girls than in men.
Cystitis is also known as a lower urinary tract infection as it occurs lower in the urinary tract system than other infections.
PLEASE NOTE: Inflammation in the bladder is called 'cystitis', whether or not it is caused by infection. If one or both kidneys are involved then the condition is called nephritis. If pain is the predominant symptom interstitial cystitis may be considered.
UTI in Women: Symptoms of Cystitis
In adults, symptoms (mild to severe) of bladder infection (cystitis or urethritis), often discribed as lower urinary tract infection, include:
- back pain, usually mid-way up the back on one side, even when not urinating;
- lower stomach, abdominal pain (over bladder), especially during urination;
- an uncomfortable pressure above the pubic bone, often experienced by women;
- abnormal urine color - dark, cloudy or milky;
- foul or strong urine odor (stinky urine);
- blood in the urine - bloody, pink urine (hematuria);
- inability to urinate - despite the urge, only a small amount of urine is passed;
- slight fever - mild infections often will not cause fever, but moderate to severe bladder infections that involve the kidneys do cause fever;
- painful or uncomfortable sexual intercourse;
- malaise (general discomfort);
- fatigue - feeling bad all over (tired, shaky, washed out);
- mental changes or confusion - in elderly people, mental changes or confusion are often the only signs of a possible urinary tract infection.
PLEASE NOTE: These symptoms do not necessarily mean there is a bladder infection. They just mean there might be a bladder infection.
UTI in Women: Incontinence
Urinary tract infections also can be one of the risk factors for a urinary bladder problem such as incontinence - leakage of urine that interferes with your normal activities, often causing embarrassment or discomfort in social situations.
Incontinence, however, is not a disease, but rather a symptom of another condition involving the urinary system, such as bladder infection.
A wide range of medical conditions, and even aging, can cause or contribute to incontinence. Some causes, such as urinary tract infections, may be temporary. Others can be long-lasting, such as:
- overactive bladder muscle,
- weakness of the muscles holding the bladder in place, or
- weakness of the sphincter muscles surrounding the urethra.
Urinary incontinence can have a varying impact on peoples lives, in many cases it can be very distressing and embarrassing, often preventing one living a normal life. This embarrassment prevents many people seeking help, this is a pity as there are many things that can be done to help.
Bladder Irritation: Noninfectious Cystitis
A noninfectious cystitis, also called abacterial, radiation or chemical cystitis, is usually assumed when no bacteria can be identified as the cause of the symptoms.
In other words, it is an irritation of the bladder not caused by a urinary tract infection with the symptoms similar to those caused by a urinary tract infection.
The exact causes of noninfectious cystitis, the most common type of cystitis in women of childbearing years, are often unknown. However, they may include:
- radiation therapy to the pelvis area,
- chemotherapy medications, and
- other irritants, such as bubble baths, feminine hygiene sprays, sanitary napkins, and spermicidal jellies,
Interstitial Cystitis/Painful Bladder Syndrome (IC/PBS)
The symptoms of a bladder infection can be mimicked by a chronic bladder disorder called interstitial cystitis (IC), also known as painful bladder syndrome (PBS). As a matter of fact, over two-thirds of all IC sufferers have a history of bladder infections.
In this disorder the bladder is overly sensitive. The major symptoms are:
- pain in the pelvic area (the lower abdomen, urethra or vagina) - the predominant symptom;
- urgent need to urinate often (up to 60 times a day).
For women who have interstitial cystitis (IC), having sex may be painful. The pain and urgency can be so severe that may make work, sexual activity and normal social functioning difficult or impossible.
Interstitial cystitis may stay about the same or get worse with time. Some people may go into remission for extended periods.
Unlike ordinary bladder infections, the cause or, rather, the causes of interstitial cystitis continue to baffle medical researchers. It is believed that IC may be the result of:
- vascular (blood vessel) disease,
- autoimmune disease,
- an acid-alkali imbalance brought about by environmental factors and diet,
- presence of abnormal substances in the urine,
- an infection caused by a more elusive strain of bacteria, undetected by standard tests,
- nerve function disorders,
- defective cells in the bladder lining, and
- allergic reactions.
Interstitial cystitis is most common in women, but it also occurs in men and children. Currently, an estimated 700,000 - 1 million Americans suffer from this disease.
UTI in Women: Other Conditions
Other conditions that have symptoms similar to urinary tract infection are:
- bladder cancer
- gonorrhea
- irritable bladder
- vaginal infection (vagina or vulva).
Excruciating pain across the abdomen or the back may signal the presence of kidney stones.
Therefore, you are strongly advised to act at the onset of any of these symptoms rather than take the "wait-and-see" approach. A professional diagnosis is essential.
Bladder Dysfunction: Diabetes
The incidence of the urologic complications of diabetes, such as autonomic neuropathy affecting the urinary bladder, ranges from 27 percent to 85 percent.
|
Diabetes mellitus presents a major health care problem in the United States. A common complication of diabetes is neuropathy: 30 percent to 70 percent diabetics are affected, depending on the neuropathy criteria.
In addition to autonomic bladder dysfunction, there is an increased incidence of asymptomatic and symptomatic bacteria, which can progress to kidney infection and kidney damage.
This increase in bladder infection in diabetes has been attributed to numerous etiologies, such as
- incomplete bladder emptying,
- changes in bladder cell wall components, and
- immune dysfunctions in the urothelial cells.
However, there are very few published research studies which address either the clinical aspects of bladder dysfunction in the diabetic or the basic molecular and cellular aspects of the diabetic bladder.
Irritable Bladder Syndrome (IBS)
The symptoms of irritable bladder are basically the same as intersticial cystitis/painful bladder syndrome (IC/PBS). Yet again the main symptoms are:
- frequency (having to urinate more often),
- urgency (not being able to wait to urinate),
- bladder discomfort or pelvic pain,
- bladder instability (the bladder tries to empty before it has filled, and you cannot control it; children, for example, may do a "potty dance" where they will suddenly squat or dance around when they need to urinate),
- nocturia (a frequent need to urinate at night).
Frequent emptying of the bladder can become a habit and this habit prevents the bladder from filling to its true capacity. It causes the bladder to become even more irritable and a vicious circle is established.
However, you can retrain your bladder by holding on by contracting your pelvic floor muscles. If "holding on" is difficult, you can try distracting your attention from your bladder by doing something. The feeling of urgency will subside as the bladder contraction dies away.
Learn to hold your urine for longer periods. Start by choosing a time interval you are reasonably comfortable with.
People with painful bladder syndrome/insterstitial cystitis often find avoiding acids and caffeine in their diet helpful, as they can trigger flare ups of symptoms.
UTI in Women: Kidney Infection (Pyelonephritis)
This is a bacterial infection (or inflammation) of the kidneys, also known as an upper urinary tract infection, as it occurs higher up in the urinary tract system than other infections.
Occasionally the bacteria causing a bladder infection with ascend up into the kidneys and cause a kidney infection. This can be serious, since kidney infections can scar the kidneys.
More likely to get a kidney infection are women who have recurrent urinary tract infections.
Fortunately, most bladder infections do not turn into kidney infections, and a small scar in one kidney infection is harmless.
But kidney infections are to be taken very seriously and treated promptly. Left untreated, a kidney infection can lead to reduced kidney function and, in severe cases, possibly even to death.
Symptoms of Kidney Infection
Here are signs, mild to severe, that a bladder infection has turned into a kidney infection:
- all symptoms of cystitis - see the above;
- lower back pain (below the ribs) or side pain - mid-way up the back, this is where the kidneys are located;
- high fever accompanied by shaking chills and sweats - an indication of a possible kidney infection; unlike "viral infections" in which the fever fluctuates between normal and very high, with kidney infections the fever stays high (usually 101º F or higher) and you look and act progressively sicker;
- nausea and vomiting - common symptoms when a kidney infection is present.
UTI in Women: Medical Diagnosis
The only way to diagnose an infection is checking a urine sample.
Urinary Analysis (U/A)
This test is commonly performed in the doctor's office or in lab. It just takes a few minutes - a dipstick is placed in the urine sample and up to ten different substances can be detected.
If the U/A is normal, and the symptoms are mild, then you can probably wait for the next few days. To be sure, a doctor can send a urine culture to the lab (see below). Therefore, you should call your doctor's office after one or two days to check the results. If positive, do not wait and call the next day again to check the sensitivity of the antibiotics (see below).
If the U/A is positive for infection, and the symptoms are moderate to severe, probably a urine culture will be sent to the lab to confirm. A doctor will start an antibiotic treatment now to avoid allowing the infection to get worse.
If the U/A is positive, but the symptoms are mild, a doctor may not start an antibiotic treatment while the urine culture is being done (since a positive U/A does not necessarily mean there is an infection).
Microscopic Urinalysis ((U/A micro)
A doctor may also wait a few hours for the lab to run a microscopic urinalysis - a drop of urine is examined under a microscope - to help in the decision whether or not to start an antibiotic treatment while the urine culture is running.
Urine Culture
With no doubt, urine culture is the most accurate test to determine for sure whether or not an infection is present.The lab puts the urine sample in an incubator. If any bacteria are in the sample, they will multiply and show up. However, it takes 24 to 48 hours for the bacteria to grow enough to be detected.
Antibiotic susceptibility testing (AST)
If only one type of bacteria grows in the culture, the lab will expose the bacteria to a variety of antibiotics to see to which ones the bacteria are sensitive. This usually takes one day after the culture is positive. It helps to decide which antibiotic is best for the infection.
PLEASE NOTE: Some microbes, like Chlamydia and Mycoplasma, can only be detected with special bacterial cultures. These infections are suspected when you have symptoms of an infection and pus in the urine, but a standard culture fails to grow any bacteria.
UTI in Women: Common Causes
|
|
In most cases, about 80 percent in adults, urinary tract infection is caused by a variety of pathogens (infectious bacteria) normally present in the intestines, especially in the rectum (colon).
Nearly all infections of the lower urinary tract and bladder are caused by a few strains of E. coli bacteria, called uropathogenic Escherichia coli (UPEC).
| |
A variety of other Enterobacteriaceae and Gram-positive pathogens, includes:
- Staphylococcus saprophyticus - 5 to 15 per cent cases of urinary tract infections,
- Group B streptococcus - bacteria that can be found in the digestive tract, urinary tract, and genital area of adults,
- Chlamydia trachomatis - one of the most common cuases of bladder infection, especially urethritis,
- Mycoplasma hominis,
- Klebsiella pneumoniae,
- Enterococcus faecalis,
- Proteus mirabilis, or
- Pseudomonas aeruginosa.
These bacteria tend to remain limited to the urethra and reproductive system and, unlike E. coli, they are sexually transmitted. However, Pseudomonas aeruginosa is the third leading cause of hospital-acquired urinary tract infections, accounting for approximately 12 percent of all infections of this type. They are usually related to urinary tract catheterization, instrumentation or surgery.
Pseudomonas aeruginosa appears to be among the most adherent of common urinary pathogens to the bladder uroepithelium. An infection can occur via an ascending or descending route.
Pseudomonas aeruginosa can also invade the bloodstream from the urinary tract. This route is the source of approximately 40 percent of pseudomonas aeruginosa infections.
Other possible causes of urinary tract infections include:
- yeast infection, especially if taking antibiotics for repeated infections,
- allergies, mainly from foods,
- stress and anxiety,
- sexual intercourse (it is common for women to get UTI's after having sex; wiping off with antibacterial wipes or washing with soap and water before and after sex is recommended),
- lubricated condoms (many women are sensitive to the spermicides),
- heavy metal toxicity, and
- poor kidney function.
Sexually Transmitted Chlamydia Infection
Chlamydia is a common sexually transmitted disease caused by a bacterium called Chlamydia trachomatis. In women, the chlamydia organism infects cells of the lining of
- the cervix,
- rectum, and
- eye.
Persons with chlamydia infections often have no symptoms. Consequently, they may transmit the infection to other people without knowing it. However, when the symptoms do occur, their type and severity will depend on the site of the infection and the person's response to it.
Women who do have symptoms of chlamydia infection may notice:
- an increased vaginal discharge,
- irritation of the area around the vagina, or
- burning pain with urination.
To diagnose chlamydia, a special test must be done by a health professional. This serious condition requires prompt medical attention.
Chlamydia infection is easily treated with an antibiotic medication. However, if it is not detected and treated, chlamydia infection can lead to complications, such as pelvic inflammatory disease, a condition that signals the infection has spread to the uterus and fallopian tubes.
Symptoms of pelvic inflammatory disease include:
- lower abdominal pain,
- painful intercourse,
- irregular periods,
- spotting and
- fever.
In pregnant women, chlamydia infection can be passed on to their newborn children, where it can cause:
- eye infections and
- pneumonia.
UTI in Women: E. Coli Infection
E.coli bacteria. An undated file photo from the USDA
|
Various harmless strains of uropathogenic E. coli (UPEC) are normally
present in the body - but they do not belong in the urinary tract.
These bacteria, however, have multiple little hairs called cilia that function like little feet that allow them to climb from the skin around the vagina, up the urinary tube, into the bladder.
If UPEC (E. coli) get into the bladder or the urethra (tube that carries urine from the bladder), the body has ways of fighting them off - including the obvious methods of simply flushing them out with the urine. But these bacteria have evolved ways of anchoring themselves to the cells of the urinary tract.
The invading E. coli bacteria take advantage of receptors naturally found on the cells of the mucosal lining of the urinary tract. These receptors are like molecular "docking bays" for substances which the cells need for their normal growth and development.
Like pirates in an old movie, E. coli use "grappling hooks", called type I pili, to first hook on to these receptors, and then to invade the cell. These pathogenic "grappling hooks" are composed of long, fibrous chains of a molecular "glue" called adhesin.
Once inside the cell, E. coli can live and reproduce in safety, shielded from many of the body's defensive immune responses.
In fact, they are so sophisticated that when the body detects that cells have been infected and activates the cell suicide program to destroy the bacteria, UPEC can actually flee the dying host cell before it is flushed out, and look for new cells to invade!
Survival Rate of E. Coli
E. coli return in as many as 30 percent of women apparently cured by antibiotics!
Bacteria E. coli are able to survive antibiotic treatment for bladder infections by reverting to an inactive state.
Within several days of antibiotic treatment, the number of bacteria reproducing drop to zero. Not all the bacteria are killed, though.
About 3 percent of the bacteria may be still present in a dormant state after treatment with ciprofloxacin (Cipro) and about 7 percent may linger after treatment with trimethoprim-sulfamethoxazole (Bactrim/Septra).
Even after a month of antibiotic exposure, about 10 million of the original 1 billion bacteria may remain.
Antibiotic treatment does not successfully kill all the bacteria participating in the infection and may. In fact, it encourages many of the bacteria to persist in a resting state.
Therefore, current standard drug treatments for bladder infections are not adequate and this phenomenon may account for many of the repeat urinary tract infections.
New Antibiotic-Resistant Strain of E. Coli
A newly identified, antibiotic-resistant strain of a common E. coli bacterium is contributing to an increase in relatively hard-to-treat bladder infections in women.
The analyzed strain, resistant to trimethoprim-sulfamethoxazole, a popular two-drug combination, shows a pattern of resistance to multiple antibiotics and has genetic characteristics called "virulence factors" that increase its ability to infect the urinary tract.
Not much is known about how new strains of bacteria that infect the urinary tract arise and spread. There is also no evidence that the new strain of E. coli is causing any increase in kidney infections or other serious complications.
It could be that this organism has been around forever and has now acquired resistance to several antibiotics. It could have been introduced, perhaps through contaminated food.
Repeated Bladder Infections
For women who are more prone to repeated infections, it can be a painful and frustrating battle.
Most likely these are women over the age of 55 years or between the ages of 25 and 29.
Those women are likely to continue having urinary tract infecions, who have had three or more a year. Therefore, they can get another infection within 18 months of the last one, or even more requently.
One possible factor behind recurrent urinary tract infection may be the ability of bacteria to attach to cells lining the urinary tract.
The symptoms sometimes can be caused by chemical irritation such as bath additives and washing powders; they may disappear if toiletries and washing powder are changed.
Usually, the latest infection stems from a strain or type of bacteria that is different from the infection before it, indicating a separate infection.
Even when several urinary tract infections in a row are due to E. coli, slight differences in the bacteria indicate distinct infections.
However, some women have recurrent symptoms suggestive of urinary tract infection - but without infection being present. This condition is not serious but can be troublesome.
Chronic or recurrent urinary tract infections should be treated thoroughly because of the chance of kidney infection (pyelonephritis).
UTI in Women: Standard Antibiotic Treatments
In the United States alone, 11 million women each year are given antibiotics for urinary tract infections. However, standard, conservative approaches to this problem are numerous and diverse.
Typically, women who have frequent recurrences (three or more a year) are offered antibiotic treatments, such:
- low doses of antibiotics for long periods of time (as long as 6 months to 2 years),
- single doses of antibiotics after sexual intercourse,
- short courses (1 or 2 days) of antibiotics when symptoms appear.
Usually, stronger antibiotics are given than for single, acute episodes of bladder infection (cystitis); after acute symptoms have subsided, prophylactic, or preventive, therapy with low-dose antibiotics is recommended.
Besides antibiotics, normally employed in a trial and error fashion with varying degrees of success, medical treatments also include:
- antidepressants to effect a change in the bladder lining,
- water dilation of the bladder,
- surgery - up to (and including) bladder removal.
UTI in Women: Doctors' Choices of Antibiotics
As urinary tract infections are extremely common, particularly in women, doctors in the United States write 2.45 million antibiotic prescriptions to treat them each year.
Almost all antibiotics will work for urinary tract infection. However, over the past 10 years, fewer doctors prescribe, for exapmle, a 10-day course of generic Bactrim or Septra, recommended by the Infectious Disease Society of America.
Bactrim and Septra
Septra and Bactrim are both brand names for a combination antibiotic called trimethoprim-sulfamethoxazole.
Trimethoprim and sulfamethoxazole are both compounds that block the internal production of folic acid (folate) needed by most bacteria to survive. These compounds, relatively safe for humans, are lethal to many bacteria.
Unfortunately, this inexpensive and quite effective, standard antibiotic for bladder infections is notorious for developing rash and allergies to it, frequently, life-threatening allergies. It is one of those famous sulfur drugs to which people have adverse reactions.
Other side effects have been reported in virtually every organ system in the body, including the kidneys. Sulfa drugs may precipitate in the urine, producing crystals that can cause bleeding, urinary obstruction,
or kidney damage.
Septra also interacts with Dilantin, with methotrexate, and with anticoagulant medications; it should be used cautiously if these other
drugs are being taken.
Generic Bactrim also tends to disrupt the intestinal bacteria more than other drugs, such as Macrobid, and cause stomach upset.
Keflex and Macrodantin
These alternatives to Septra and Bactrim are commonly used both for the active treatment and long-term prevention of urinary tract infections. They seem to be more effective and even safer than Septra, although
each carries risks of its own.
As you can see, in prescribing antibiotics, the risks and benefits must be always balanced!
Cipro and Marcrobid
The majority of doctors opt for newer (and more expensive) antibiotics, such as Cipro (a type of fluoroquinolone) or Marcrobid.
An often-prescribed by obstetricians generic Marcrobid tends to have minimal negative effect on the intestine, as most of this drug is concentrated in the bladder.
This trend may be due to doctors, adopting a new drug, believing it is the better drug. Therefore, it runs counter to the formal recommendations for drugs to be used first, such Bactrim, in the treatment of urinary tract infections.
There are also differences between the medical specialties in prescribing antibiotics:
- internists are most likely to prescribe fluoroquinolones, such as Cipro, and
- obstetricians are most likely to prescribe nitrofurantoin, such as Marcrobid.
Ciprofloxacin (Cipro) Therapy: Adverse Reactions
Just in the U.S., antibiotics cause 700,000 emergency room visits per year. (Associated Press, Oct. 17, 2006)
|
The reported serious adverse effects - temporary and/or permanent - that may occur and manifest during fluoroquinolone (ciprofloxacin) therapy and long after it had been discontinued, include:
- irreversible peripheral neuropathy (damage to nerves of the peripheral nervous system),
- spontaneous tendon rupture and tendonitis (inflammation of a tendon),
- acute liver failure or serious liver injury (hepatitis),
- Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) - also known as Lyell's syndrome, considered a more severe form of Stevens-Johnson syndrome (rare, life-threatening dermatological conditions characterized by the detachment of the top layer of skin from the lower layers of the skin all over the body),
- severe central nervous system disorders,
- Clostridium difficile associated disease (pseudomembranous colitis, an infection of the colon), a cause of antibiotic-associated diarrhea (AAD),
- photosensitivity/phototoxicity reactions,
- psychotic reactions and confusional states,
- acute pancreatitis (inflammation of the pancreas),
- bone marrow depression or myelotoxicity (affecting the immune system),
- interstitial nephritis (inflammation of the kidneys),
- hemolytic anemia (anemia due to the abnormal breakdown of red blood cells),
- loss of vision,
- irreversible double vision (diplopia),
- drug-induced psychosis (loss of contact with reality),
- chorea (involuntary muscle movements),
- impaired color vision,
- exanthema (rash),
- abdominal pain,
- malaise (feeling of being unwell),
- drug-induced fever,
- dysaesthesia (unpleasant, abnormal sense of touch),
- eosinophilia (elevated white blood cells count),
- pseudotumor cerebri (PTC), commonly known as idiopathic intracranial hypertension (IIH), also referred to as increased intracranial pressure (pressure around the brain).
NOTE: The elderly are at a much greater risk of experiencing such adverse reactions during fluoroquinolone therapy and long after it had been discontinued.
UTI in Women: Limitations of the Antibiotic Treatments
In 15 percent of cases, bladder or kidney infections can become a recurring problem, or they can stop responding to the antibiotics.
|
Unfortunately, bacteria can survive after antibiotic treatment. For example, bladder infections caused by a common bacterium E. coli return in as many as 30 percent of women apparently "cured" by antibiotics.
Bacteria E. coli are able to survive antibiotic treatment for bladder infections by reverting to an inactive state.
Although, within several days of antibiotic treatment, the number of bacteria reproducing drop to zero - NOT ALL the bacteria are killed.
For example, after treatment with ciprofloxacin (Cipro)
- about 3 percent of the bacteria may be still present in a dormant state.
After treatment with trimethoprim-sulfamethoxazole (Septra and Bactrim)
- about 7 percent of the bacteria may still linger.
Even after a month of antibiotic exposure, about 10 million of the
original 1 billion bacteria may remain.
It is a well-known fact that antibiotic treatments:
- do NOT successfully kill all the bacteria participating in the infection and
- may, in fact, encourage many of the bacteria to persist in a resting state.
Therefore, current standard drug treatments for bladder infections are not adequate and this phenomenon may account for many of the repeat urinary tract infections. In 15 percent of cases, bladder or kidney
infections can become a recurring problem, or they can stop responding to the antibiotics.
UTI in Women: Drawbacks of the Antibiotic Treatments
Although routinely used, antibiotic treatments have many drawbacks, such as:
- antibiotics successfully kill both the unwanted micro-organisms and wanted micro-organisms;
- long-term or often repeated antibiotic use leads to major disturbance in normal body microflora, and sometimes to major disruption in health;
- antibiotics, such as Bactrim, may cause stomach upset, rash, and allergic reactions;
- many women end up with nasty yeast infections; as the friendly bacteria are killed off along with the bad bacteria, the antibiotic insensitive yeast can then grow out of control.
Therefore, due to the hazards, especially of prolonged antibiotic therapy, the need for antibiotics used to clear up the infection, should be reduced, as ALL antibiotic therapies carry with them the risks of developing:
- antibiotic-resistant bacteria,
- gastrointestinal problems, and
- adverse effects, especially on the liver and kidneys.
Urinary Self-Defense Systems Against Bacteria
Infection does not always occur when bacteria are introduced into the bladder because the urinary system is structured in a way that helps ward off infection.
A number of defense systems - natural safeguards - that protect the urinary tract against infection-causing bacteria includes:
- The flow of urine which functions as an antiseptic, helping to wash potentially harmful bacteria out of the body during normal urination. (Urine is normally sterile, that is, free of bacteria, viruses, and fungi!).
PLEASE NOTE: Urine contains large quantities of urea - the colorless, crystalline end product manufactured within the liver - which is excreted from the body via urinary tract. Known for its antiseptic and bactericidal properties, urea helps to inhibit the growth of many types of detrimental bacteria including Eschericia coli (E. coli) and Staphylococcus. Also present in the skin where it functions as one of the endogenous components of the skin's natural moisturizing factor, urea helps to kill the detrimental bacteria that cause bacterial forms of prostatitis.
- The ureters (tubes that carry urine from the kidneys to the bladder) and bladder which are structurally designed to prevent urine from backing up toward the kidneys;
- The immune defenses in both sexes continuously fights bacteria and other harmful micro-invaders. In addition, immune system defenses and antibacterial substances in the mucous lining of the bladder eliminate many organisms;
- The vagina which is colonized - in normal fertile women - by lactobacilli, beneficial micro-organisms that maintain a highly acidic environment (low pH). Acid is hostile to other bacteria. Lactobacilli also produce hydrogen peroxide, which helps eliminate bacteria and reduces the ability of E. coli - the major bacterial culprit in urinary tract infections - to adhere to vaginal cells;
- The bladder lining - when bacteria infect the cells that line the bladder they, literally, sacrifice themselves and self-destruct (a process called apoptosis). In so doing, they fall away from the lining, carrying the bacteria with them. This process, sugested by some interesting research, eliminates about 90% of the E. coli;
- A possible natural antibiotic - identified by some researchers - called human beta-defensin-1 (HBD-1) which fights E. coli within the female urinary and reproductive tracts.
UTI in Women: Common Risk Factors
There is a number of factors that increase the risk of developing urinary tract infection - some women are more prone to getting an infection than others:
Being Female
The female urethra is shorter than the male's, allowing bacteria quick access to the bladder and this probably accounts for why women are more likely to develop urinary tract infection. In addition, a woman's urethral opening is near sources of bacteria from the anus and vagina.
Being Pregnant
Pregnant women, especially in the late stages of pregnancy, seem no more prone to an infection than other women; however, about 5 to 7 percent of pregnant women develop a urinary infection, probably due to previous infections before pregnancy, high sexual activity and diabetes, and also due to hormonal changes and shifts in the position of the urinary tract during pregnancy (the enlarged uterus continuously presses on the bladder).
PLEASE NOTE: Women who experience an untreated urinary tract infection during their third trimester of pregnancy are at greater risk of delivering a child who suffers from mental retardation or developmental delay.
Poor Hygiene
Genitals must be kept dry and clean! Less than careful hygiene, especially after developing loose stools or diarrhea, is one of the most frequent causes of repeated urinary tract infections.
It is very easy to contaminate one's fingers when wiping oneself with toilet paper, and if those contaminated fingers come anywhere close to the opening of the urethra, there is a high likelihood of infection in predisposed individuals.
Only white unscented toilet paper should be used as many women react to the dyes and chemicals in the other toilet papers. Unbleached toilet paper would be even better to reduce any possible chlorine exposure and the environmental contamination that comes from the bleaching process.
Dehydration
Not drinking enough water can increase the risk of urinary tract infections. Dark-yellow urine and/or infrequent urination are the symptoms of dehydration. To prevent dehydration, adult women should consume around six to eight cups of fluids or beverages each day.
Many women, however, believe that drinking water causes fluid retention. In fact, the opposite is true. The body retains water only if there is two little water is the cells.
Unfortunately, we seldom think of water as an essential, vital nutrient and don't realize the important part it plays in major body functions.
Sexual Position
Some women find that they are liable to develop an infection if, during sexual intercourse, their partner enters their vagina 'from behind'. This is simply because in this position it is more likely that bacteria from around the anus may be pushed forward towards the urethra.
Diaphragm Use
Some women who use a diaphram are likely to develop a urinary tract infection; also women whose partners use a condom with spermicidal foam also tend to have growth of E. coli bacteria in the vagina, which may enter the urethra.
Frequent Intercourse: Honeymoon Cystitis
In some women, high sexual activity may traumatize the urethra, disrupting its lining and making it more susceptible to infection. This is frequently called honeymoon cystitis.
The Elderly
If you are an older adult you are at high risk for developing bladder infection (cystitis), with the incidence being as high as 33 out of 100 people.
What may place the elderly at increased risk for developing bladder infection, is
- lack of adequate fluids,
- bowel incontinence,
- decreased mobility or immobility, or
- placement in a nursing home (a stress factor).
Postmenopausal
In postmenopausal women usually vaginal tissues start to break down due to a decrease in estrogen levels; therefore, in general, the rate of urinary tract infections gradually increases with age.
Urinary Incontinence
Urinary tract infection also can be one of the risk factors for a urinary bladder problem such as incontinence - leakage of urine that interferes with some of your normal activities, often causing embarrassment or discomfort in social situations.
However, incontinence is not a disease, but rather a symptom of another condition involving the urinary system, such as acute or frequent bladder infections.
A wide range of medical conditions, and even aging, can cause or contribute to incontinence. Some causes, such as urinary tract infections, may be temporary.
Urinary incontinence can have a varying impact on peoples lives, in many cases it can be very distressing and embarrassing, often preventing one living a normal life. This embarrassment prevents many people seeking help, this is a pity as there are many things that can be done to help.
Failure to Completely Empty the Bladder
This failure is associated with such conditions, mainly obstructions, as:
- kidney stones,
- tumor,
- urethral strictures, or
- neurological diseases.
Urinary Tubes, Stents, or Catheters
An obstruction in the urinary tract can be due to:
- nephrostomy tubes (a tube inserted into the kidney to drain urine to the abdominal surface), or
- ureteric stents (a wire tube fitted in the urethra to keep the passage open) all tend to increase the likelihood of infection, or
- urinary catheters (a small tube inserted into the bladder through the urethra to drain urine) - a usual cause of urinary tract infection due to bacteria on the catheter, especially in the elderly or those who lose bladder control, or are unconscious, or are critically ill (due to nervous system disorder).
PLEASE NOTE: Catheterization in males is more difficult and uncomfortable than in females because of the longer urethra.
Diabetic Bladder
Diabetics are at a higher risk of a urinary tract infection due to the unfavourable metabolic changes, especially the elevated blood sugar levels, which suppress their immune system.
The incidence of the urologic complications of diabetes, such as autonomic neuropathy affecting the urinary bladder, ranges from 27 percent to 85 percent.
In addition to autonomic bladder dysfunction in diabetes, there is an increased incidence of asymptomatic and symptomatic bacteria, which can progress to kidney infection and kidney damage.
This increase in bladder infection in diabetes has been attributed to numerous etiologies, such as:
- incomplete bladder emptying,
- changes in bladder cell wall components, and
- immune dysfunctions in the urothelial cells.
However, there are very few published research studies which address either the clinical aspects of bladder dysfunction in the diabetics or the basic molecular and cellular aspects of the diabetic bladder.
Neurogenic Bladder: Paraplegia, Quadriplegia (SCI)
Neurological conditions like paraplegia, a spinal cord injury, also called spinal cord impairment (SCI), usually result in neurogenic bladder - an unstable or atomic bladder, with no muscle tone.
People with spinal cord injuries have lost, partial or complete, control over their bladder and sphincter due to the compromised nerve receptors that are responsible for:
- contracting and relaxing the muscles of the bladder and the sphincter, and
- registering feelings of pressure or release.
Due to this condition, most paraplegics are exposed to the regular use of catheters and drugs. (The more traditional cap and bag, with continual drainage, is falling from favor even though it is a safer system).
However, catheters often increase the risk of urinary tract injuries and repeated bladder infections - a common problem in people with spinal cord impairment.
Exposed to repeated or long-term courses of antibiotics, in time, they also develop resistance to drugs what makes maintaining healthy urinary tract for them even more difficult.
However, contrary to a popular belief and common medical practice, men with spinal cord injuries or spinal cord impairment do NOT have to:
- suffer from chronic bladder infections,
- be exposed to vicious antibiotics.
Childhood Urinary Tract Infections
A history of urinary tract infections or bladder infections in childhodd also poses a risk for recurrences in adult life.
Congenital Abnormality: Vesico-Ureteric Reflux
Abnormal structure of the bladder can be something that you are born with
or that develops later in life. Vesico-ureteric reflux is a congenital abnormality of the urinary tract that some children are born with, in which urine flows back into the ureters or kidney during urination.
Suppressed Immune System
Urinary tract infections occur when the immune system is supressed or compromised due to chronic illness, such a diabetes, AIDS, and cancer.
Blood Type
People with certain blood types attract bacteria which attach to
cells that line the urinary tract, causing recurrent urinary tract infections.
UTI in Women: Prevention Health Tips
Bladder infections occur when microbes, mainly bacteria, get through the urethra into the bladder. This can happen by the way you wipe after going to the bathroom, or through sex. Bladder infections can also be caused by a blockage of urine flow, which may occur in pregnant women.
Practice good personal hygiene by keeping the genital area clean - less than careful hygiene, especially after developing loose stools or diarrhea is one of the most frequent causes of recurrent bladder infections.
Urinate when you feel the need - do not resist the urge to urinate!
Take showers instead of tub baths.
Use only white unscented and, preferably, unbleached toilet paper - you may react to the dyes and chemicals in the other toilet papers.
PLEASE NOTE: Unbleached toilet paper would be even better to reduce any possible chlorine exposure and the environmental contamination that comes from the bleaching process.
Cleanse the genital area before
sexual intercourse - wash the vulva, penis, hands and/or dildo with soap and water prior to vaginal penetration; this will reduce the risk of introducing bowel bacteria into the vagina and urethra.
PLEASE NOTE: If condoms are used during anal contact, make sure condoms are changed.
Wipe from front to back after you go to the bathroom - it helps prevent bacteria around the anus from entering the vagina or urethra.
PLEASE NOTE: It is very easy to contaminate one's fingers when wiping oneself with toilet paper, and if those contaminated fingers come anywhere close to the opening of the urethra, there is a high likelihood of infection, especially in predisposed individuals.
Change sexual positions - choose the position that causes less friction on the urethra.
Lubricate adequatly during sexual intercourse - it will decrease urethral irritation.
Urinate AFTER sexual intercourse - do a "flush technique" within ten (10) minutes, if possible; if not, drink 10-12 ounces of water immediately after intercourse. It will cause you to urinate later and help flush the bacteria out.
Avoid wet or tight clothing - wear loose pants.
Do not wear a wet bathing suit for a long time.
Avoid nylon underwear and Spandex clothing - they promote moistness and irritation of the meatus (urethral opening); wear cotton underwear instead, it is less irritating and provides more ventilation than nylon.
Use pantyhose with cotton crotches.
Avoid chemicals such as feminine hygiene sprays, bubble baths, strong soaps and douches - they may irritate the urethra.
Evaluation of Symptoms: Questionnaire
|
If you are interested in getting a second opinion, please copy the following questions and send your answers by e-mail (click the red link below):
- For how many days has the pain when urinating been present?
- How old are you?
- What is your gender?
- Do you have fever? (Yes/No)
- Do you have back pain? (Yes/No)
- Do you have nausea? (Yes/No)
- Do you have the sudden, strong urges to urinate? (Yes/No)
- Do you need to urinate more often than usual? (Yes/No)
- Please add additional information related to your condition.
Within 48 hours, you may expect an evalution of your symptoms along
with a brief information on available natural treatment options.
|
Uribiotic Formula: Herbal Antibiotic
"As a last resort I tried URIBIOTIC, and within a few days the effects were amazing: clear, golden urine and a nice, relaxed bladder; relief at last. For this, I am most grateful and I thank you! ~ David P., Devon, UK
|
It has been known for years to alternative practitioners - nutritionists, herbalists, naturopathic doctors and nutritionally-oriented physicians that the natural, non-pharmacological approach to urinary tract infection (UTI for short) compared to standard medical treatments (read: antibiotics) is clearly a superior, and most importantly, safer and without side effects option.
Actually, it is on open secret that antibacterial and anti-inflammatory herbs, micro- and phytonutrients can help to remedy and overcome acute and repeated, chronic bladder infections by:
- disinfecting the urinary tract (an antimicrobial action),
- inhibiting and preventing inflammation,
- enhancing the growth of some forms of beneficial bacteria within the body such as Bifidobacteria bifidus and Lactobacillus acidophilus,
- destroying some forms of detrimental fungi such as Candida albicans and Candida krusei.
By preventing bacterial cell division and breaking down the walls and cytoplasm of bacteria (in a similar fashion to some types of pharmaceutical antibiotics), Uribiotic Formula helps to inhibit the growth (or kill) many types of detrimental pathogenic bacteria including:
- Actinomyces naeslundii
- Bacillus anthracis (on the basis of its known ability to kill other species of Bacillus)
- Bacillus alvert
- Bacillus cereus
- Bacillus subtilis
- Brucella abortus
- Campylobacter jejuni
- Chlamydia pneumoniae
- Chlamydia trachomatis
- Citrobacter freundii, a species of motile, gram-negative Citrobacter - a genus of gram-negative coliform bacteria in the Enterobacteriaceae family. Citrobacter bacteria can be present in the intestines, feces, soil, water, urine, sewage and food; they are also the source of infant meningitis and sepsis.
Citrobacter freundii strains have inducible ampC genes encoding resistance to ampicillin and first-generation cephalosporins.
- Clostridium species (botulinum, tetani)
- Cornybacterium diphtheriae
- Enterobacter aerogenes, gram-negative aerobe, also known as Klebsiella mobilis or Klebsiella aerogenes (the latter at one time was used for several strains now known to belong to Klebsiella pneumoniae; now it is used primarily by researchers who believe that Enterobacter aerogenes should be transferred to Klebsiella).
- Enterococcus faecalis (gram-positive aerobe, former Group D streptococcus)
- Eschericia coli (E. coli, gram-negative aerobe)
- GBS, see Streptococcus agalactiae
- Helicobacter pylori (H. pylori)
- Haemophilus influenzae
- Klebsiella pneumoniae (gram-negative aerobe)
- Legionella pneumoniae
- Listeria monocytogenes
- Moraxella catarrhalis
- Mycobacterium smegmatis
- Mycobacterium tuberculosis
- Mycoplasma hominis (see: Ureaplasma urealyticum)
- Neisseria gonorrhoeae
- Neisseria memingitidis
- Pasteurella septica
- Pneumocystis carinii
- Propionibacterium acnes
- Proteus mirabilis (gram-negative aerobe)
- Proteus vulgaris (gram-negative aerobe)
- Pseudomonas aeruginosa (gram-negative aerobe)*
- Pseudomonas cepacia
- Salmonella enteridis
- Salmonella enteritidis
- Salmonella choleraesuis
- Salmonella paratyphi A
- Salmonella typhimurium
- Serratia marcescens (gram-negative aerobe)
- Shigella dysenteriae
- Shigella flexneri
- Shigella sonnei
- Staphylococcus aureus (gram-positive aerobe, responsible for "Golden Staph")**
- Staphylococcus saprophyticus (a gram-positive, coagulase-negative bacterium, recognized as a cause of urinary tract infections since the early 1970s)
- Streptococcus agalactiae (also known as group B streptococcus or GBS) is a gram-positive coccus anaerobe. Although a harmless commensal bacterium being part of the human microbiota in the genitourinary tract of up to 30% of healthy human adults, it can cause severe invasive infections, such as urinary tract infections, especially in the elderly and individuals compromised by underlying diseases such as diabetes. Sometimes, it can cause serious illness for the mother and the baby during gestation and after delivery. GBS urinary tract infections may also induce labour and cause premature birth. Penicillin is the antibiotic of choice for treatment.
- Streptococcus faecalis (now classified as Enterococcus faecalis)
- Streptococcus Group B, see Streptococcus agalactiae
- Streptococcus mutans (alpha-hemolytic Streptococcus), also known as Group A Streptococcus (GAS)
- Streptococcus pneumoniae (alpha-hemolytic Streptococcus), also known as Group A Streptococcus (GAS)
- Streptococcus pyogenes (beta-hemolytic Streptococcus), also known as Group A Streptococcus (GBS)
- Streptococcus sanguis (alpha-hemolytic Streptococcus), also known as Group A Streptococcus (GAS)
- Streptococcus viridans (alpha-hemolytic Streptococcus), also known as Group A Streptococcus (GAS)
- Streptomyces species
- Treponema pallidum
- Ureaplasma urealyticum - a species of detrimental ureaplasma bacteria, a genus of bacteria belonging to the family Mycoplasmataceae. Mycoplasma, also known as Asterococcus, is a genus of aerobic to facultatively anaerobic, gram-negative detrimental bacteria. Several species are pathogenic in humans, including Mycoplasma fermentans, Mycoplasma genitalum and Mycoplasma pneumoniae.
U. urealyticum - the phylogenetic cluster of M. pneumoniae, is part of the normal genital flora of both men and women. It is found in about 70 percent of sexually active humans. It is believed to be sexually transmitted and transmitted from mother to infant.
Ureaplasma urealyticum infection may cause urinary tract infections (UTIs), urinary tract/kidney stones (struvite stones), non-specific urethritis (NSU), nongonorrheal urethritis and prostatitis in men. It has also been noted as one of the infectious causes of sterile pyuria (pus in urine).
Penicillins are ineffective as U. urealyticum does not have a cell wall, which is the drug's main target.
- Vancomycin-Resistant Enterococcus (VRE)
* PLEASE NOTE: Pseudomonas aeruginosa is a common bacterium found in soil, water, skin flora and most man-made environments. An opportunistic pathogen of immunocompromised individuals vulnerable to infections, it typically infects the pulmonary tract, urinary tract, burns, wounds, and also causes other blood infections.
P. aeruginosa is the third leading cause of hospital-acquired urinary tract infections, accounting for approximately 12 percent of all infections of this type. They are usually related to urinary tract catheterization, instrumentation or surgery.
It is a common cause of post-operative infection in radial keratotomy (RK) eye surgery patients and of "hot-tub rash" (dermatitis), caused by lack of proper periodic attention to water quality.
P. aeruginosa appears to be among the most adherent of common urinary pathogens to the bladder uroepithelium. An infection can occur via an ascending or descending route.
P. aeruginosa can also invade the bloodstream from the urinary tract. This route is the source of approximately 40 percent of P. aeruginosa infections.
P. aeruginosa can cause chronic opportunistic infections. These kinds of infections are a serious problem for medical care. Many patients, immunocompromised and the elderly in particular, often cannot be treated effectively with traditional antibiotic therapy.
As a highly relevant opportunistic pathogen, P. aeruginosa has low antibiotic susceptibility. It is naturally resistant to a large range of antibiotics and may demonstrate additional resistance after unsuccessful treatment.
Therefore, choosing an antibiotic should be guided according to laboratory sensitivities, rather than empirically. However, if antibiotics are started empirically - with some exceptions, given by injection only - then cultures should be obtained and, after having the culture results available, the choice of an antibiotic used should be carefully reviewed.
Thanks, Andrew, for your advice and support with my Pseudomonas [aeruginosa] bladder infection with your amazing product Uribiotic which stopped the infection and kept it away.
I've suffered from UTIs for 18 years since my spinal cord injury and now I'm infection free.
JASON C.
Great Britain
|
** PLEASE NOTE: In case of Staphylococcus aureus infections, Uribiotic Formula can be a part of a combined antibiotic therapy as it may enhance the effectiveness of pharmaceutical antibiotics for the UTI treatment.
Uribiotic Formula: An Immune Booster
An immune-boosting Uribiotic Formula helps to increase the natural safeguards - bodily defense systems that protect the urinary tract against pathogenic, infection-causing bacteria, such as:
- the flow of urine which functions as an antiseptic, helping to wash potentially harmful bacteria out of the body during normal urination. (Urine is normally sterile, that is, free of bacteria, viruses, and fungi!);
- the ureters (muscular ducts that propel urine from the kidneys to the urinary bladder) and the bladder;
- the immune defenses and antibacterial substances in the mucous lining of the bladder;
- the bladder lining cells that, literally, sacrifice themselves and self-destruct to fight off detrimental bacteria (a process called apoptosis). In so doing, they fall away from the lining, carrying the bacteria with them. This process, suggested by some interesting research, eliminates about 90% of the E. coli;
- the vagina which is colonized - in normal fertile women - by lactobacilli, beneficial micro-organisms that maintain a highly acidic environment (low pH). Lactobacilli also produce hydrogen peroxide, which helps eliminate bacteria and reduces the ability of E. coli to adhere to vaginal cells;
- the so-called human beta-defensin-1 (HBD-1) which fights E. coli within the female urinary and reproductive tracts -.a possible natural antibiotic identified by some researchers;
- the antibacterial actions of some secretions of the prostate gland probably for why men are less likely than women to develop urinary tract infection.
Uribiotic Formula: Health Benefits

|
It is so embarrassing to consult your doctor for the same reason (another infection!) and need to take another round of different antibiotics (the trial and error method of problem "solving").
The truth is, however, that urinary tract infections CAN be successfully prevented, remedied and overcome naturally - without multiple rounds of prescription medications (antibiotics).
Health benefits of our proprietary Uribiotic Formula - a synergistic blend of 60 nutrients, phytonutrients (plant nutrients) and herbs thoroughly researched and put to the test - include:
- anti-inflammatory,
- antibacterial,
- antifungal,
- antiviral,
- antiparasitic,
- antioxidant,
- diuretic,
- anti-edematous (decreasing edema and swelling), and
- antitumor.
Formulated with care by a master formulator and manufactured according to the highest standards, this unique synergistic combination can help you deal with a bladder and/or even a kidney infection:
- safely,
- effectively, and
- with no side effects.
Thousands of UTI sufferers around the world have proven the efficacy of this approach. And what is most important, there has not been a single reported harm done by taking the Uribiotic Formula.
But don't take our word for it - try it out yourself.
|
Naturopathic
Uribiotic® Formula
Advanced Urinary Tract Support*
 MADE IN USA MADE IN USA
60 Phytonutrients and Nutrients
72 Capsules
SUPPLEMENT FACTS:
Amount Per Serving (4 Capsules)
|
|
| 1. Vitamin A (All Trans Retinyl Palmitate) |
450 mcg |
| 2. Vitamin C (Calcium Ascorbate) |
60 mg |
| 3. Vitamin E (d-Alpha-Tocopherol Succinate) |
16.75 mg |
| 4. Riboflavin (Vitamin B-2) |
5 mg |
| 5. Vitamin B-6 (as Pyridoxine HCl) |
5 mg |
| 6. Biotin |
300 mcg |
| 7. Magnesium (as Taurinate) |
150 mg |
| 8. Zinc (as Monomethionine) |
25 mg |
| 9. Selenium (as Selenomethionine) |
25 mcg |
| 10-60. PROPRIETARY BLEND: |
|
| Grape Seed (Vitis vinifera) Extract (Std. to 95% Oligomeric Proanthocyanidins), Buchu Short Leaf 4:1 Extract, Oregano Leaf 5:1 Extract, Uva Ursi Leaf Extract (Std. to 20% Arbutin), Corn (Zea mays) Silk Extract, Echinacea (Echinacea angustifolia Root Extract, Echinacea purpurea Aerial Parts Extract), Horseradish (Armoracia rusticana) Root 10:1 Extract, Bee Propolis 2:1 Extract, Goldenseal Root Extract (Std. to 5% Berberine, Grapefruit (Citrus paradisi) Seed 4:1 Extract, Olive (Olea europaea) Leaf 4:1 Extract, Meadowsweet Herb Powder, Saw Palmetto Berry Extract (Std. to 25% Fatty Acids), Stinging Nettle Root 10:1 Extract, Caprylic Acid (as Sodium caprylate), Garlic Bulb Powder, Gotu Kola (Centella asiatica) Leaf Extract (Std. to 10% Asiaticoside), Purple Mangosteen (Garcinia mangostana) Rind Extract(Std. to 10% Mangostin), Cranberry (Vaccinium macrocarpon) Fruit Powder (90% Cranberry Solids), Horsetail Stem Extract (Std. to 7% Silica), Onion (Allium cepa) Bulb Powder, Pau D'Arco Bark 4:1 Extract, Watermelon (Citrullus lanatus) Fruit 4:1 Extract, Asparagus Shoot Powder, Astragalus Root Extract (Std. to 0.5% Astragalosides), Moringa (Moringa oleifera) Leaf 4:1 Extract, Black Walnut Hull Powder, Calcium D-Glucarate, Clove (Syzygium aromaticum) Bud Powder, Green Cardamom (Elettaria cardamomum) Seed Powder, N-Acetyl L-Cysteine, Pomegranate Fruit Extract (Std. to 40% Ellagic Acid), Rutin, Cayenne Fruit Powder, Cinnamon (Cinnamomum cassia) Bark 4:1 Extract, Great Yellow Gentian Root Powder, Hesperidin, Rosemary Leaf Extract (Std. to 6% Carnosic Acid), Triphala (Terminalia bellirica, Terminalia chebula, Emblica officinalis) Fruit Powder, Eleutherococcus senticosus Root Extract (Std. to 0.8% Eleutherosides), Horse-Chestnut (Aesculus hippocastanum) Fruit Extract (Std. to 20% Aeicin), Milk Thistle (Silybum marianum) Seed Extract, Bromelain, Chlorophyll (as Sodium Copper Chlorophyllin), Papain, Bergamot (Citrus bergamia) Dried Fruit Peel Powder, Trans-resveratrol, Vanadium (as V Sulfate), BioPerine® Black Pepper (Piper nigrum) Fruit Extract, Lycopene, Boron (as B Citrate). |
1,192.46 mg |
| Other Ingredients: Vegetable Cellulose (Capsule), Microcrystalline Cellulose, Vegetarian Leucine. |
|
Manufactured in the USA with domestic and imported ingredients in a GMP [Good Manufacturing Practice] Compliant Facility.
BioPerine® is a registered trademark of Sabinsa Corporation.
|
QUALITY & SAFETY
ASSURANCE |
| As a dietary supplement, starting after breakfast, take 4 capsules 3 times daily in between meals, each time with 4 ounces (½ cup) of alkaline room-temperature water, or as recommended by a qualified healthcare professional. |
SUGGESTED USE |
| If you are taking antidiabetic or thyroid medications, or have a gastrointestinal condition, consult with your healthcare practitioner before taking this product. Do not take this product if you are pregnant, nursing or planning to become pregnant. |
WARNING |
| Discontinue use 2 weeks prior to elective surgery. |
CAUTION |
| Allergen free (Milk, eggs, fish, crustacean shellfish, tree nuts, peanuts, wheat, soy). |
PREMIUM PURITY |
Uribiotic® Formula*
The Mierzejewski Formula™
Formulated and distributed by Full of Health, Inc.
Lancaster, PA 17601
1.705.304.6246
* This statement has not been evaluated by the FDA. This product is not intended to diagnose, treat, cure or prevent any disease. |
Full of Health and Uribiotic are registered trademarks of Full of Health, Inc. |
Unique, Natural and Astonishingly Effective
Our all-natural Uribiotic Formula is so astonishingly effective that it continues to amaze even the most skeptical people, including medical doctors and other health professionals. Why? Because the combination of the above active ingredients provides comprehensive and balanced support for the entire urinary tract.
For this reason, we have decided to go worldwide and share our experience with the public on the Internet to help men around the world to overcome and remedy urinary tract infection that can lead to dangerous complications, such as kidney infection.
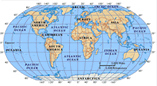 Since 2004, we have been supplying with our proprietary Uribiotic Formula clients and customers in 34 countries: the United States, Australia, the United Kingdom, South Africa, New Zealand, Germany, Belgium, Mexico, Italy, Singapore, France, Russia, Croatia, Poland, Portugal, Denmark, United Arab Emirates, Hong Kong, St. Lucia (West Indies), Norway, Saudi Arabia, Turkey, Slovenia, Greece, Qatar, Jordan, Israel, the Netherlands, Luxembourg, Sri Lanka, India, Spain, China, and Chile.
Since 2004, we have been supplying with our proprietary Uribiotic Formula clients and customers in 34 countries: the United States, Australia, the United Kingdom, South Africa, New Zealand, Germany, Belgium, Mexico, Italy, Singapore, France, Russia, Croatia, Poland, Portugal, Denmark, United Arab Emirates, Hong Kong, St. Lucia (West Indies), Norway, Saudi Arabia, Turkey, Slovenia, Greece, Qatar, Jordan, Israel, the Netherlands, Luxembourg, Sri Lanka, India, Spain, China, and Chile.
With no doubt this unique supplement can be of great benefit to you. You have nothing to lose - and your urinary health to gain.
If necessary, Uribiotic Formula can be a part of a combined antibiotic therapy as Uribiotic Formula may even enhance the effectiveness of standard pharmaceutical antibiotics for the treatment of urinary tract infections (UTIs), especially in case of Staphylococcus aureus infections.
First Signs of Relief Within 24-48 Hours
|
Uribiotic Formula can cause an almost instant disappearance of
- the painful burning sensation when urinating,
- the need for frequent urination,
- the inability to empty the bladder completely even though you have the urge.
Uribiotic Formula can help to eliminate:
- the harmful bacteria from the inside of the urinary tract without disrupting the normal body functions.
Uribiotic Formula can help you prevent and remedy:
- both acute and repeated (chronic) urinary tract infections, and
- the need and dependence on antibiotics.
The results, however, may vary from person to person depending on the type of diagnosis (urine tests and/or symptoms), the type of bacteria, degree of severity of UTI (ranging from minor to serious), type of UTI (cystitis, urethritis, pyelonephritis), history of antibiotic intake (as this can be a cause of repeated UTIs), structural abnormalities, age, sex and other existing health conditions such as diabetes mellitus and/or any immuno-compromised state. Besides, about half of women with symptoms of a UTI actually have irritation of the urethra, vaginitis, candidiasis, interstitial cystitis, or sexually transmitted diseases (STDs). Some of these problems may also accompany or lead to UTIs.
|
Appreciated by Our Satisfied Customers Since 2003
|
I have been purchasing the Uribiotic Formula for my father on behalf of my Mom for the past several months. So far, the results are amazing.
My father has a catheter and because of this has suffered numerous hospitalizations with urinary tract and bladder infections. Due to the numerous prescriptions of antibiotics, he had developed a resistance to most.
For the past few years, he has been in and out of the hospital and rehabilitation centers. This has taken a tremendous toll on him and the whole family, not to mention the financial burden.
I am happy to report that the Uribiotic Formula has been working. It's so nice to visit him and see him in good spirits.
I am so thankful to have found Uribiotic.
Theresa P.
Gilroy, California
|
|
I'm pleased to let you know that URIBIOTIC killed pseudomonas bacteria* completely!
Thank you!
Steve M.
Dublin, CA
*Pseudomonas aeruginosa is a common bacterium - the third leading cause of hospital-acquired urinary tract infections, accounting for approximately 12 percent of all infections of this type usually related to urinary tract catheterization, instrumentation or surgery.
P. aeruginosa appears to be among the most adherent of common urinary pathogens to the bladder uroepithelium. An infection can occur via an ascending or descending route. It can also invade the bloodstream from the urinary tract. This route is the source of approximately 40 percent of P. aeruginosa infections.
As a highly relevant opportunistic pathogen, P. aeruginosa has low antibiotic susceptibility. It is naturally resistant to a large range of antibiotics and may demonstrate additional resistance after unsuccessful treatment.
|
|
Hello Mr. Andrew Mierzejewski,
I am writing to thank you for all you have done for me. I had an E. coli infection ruining my life for 6 years. I had seen numerous doctors and been tested every way that the medical profession could think of.
It started on my 50th birthday when my health deteriorated rapidly within 2 hours. I was feeling fine, sitting in Northern Ontario contemplating my first 5 decades of life. I felt tired after eating lunch and thought I should take a nap. Within two hours I had a fever of 104. I was vomiting and shaking uncontrollably.
My wife called for an ambulance and I was rushed to the hospital in Bracebridge. Once there, I was diagnosed with a severe urinary tract infection. They prescribed Cipro and sent me on way. The strain of E.coli in me was resistant to that antibiotic and consequently I had another violent attack, and my second ride in an ambulance. The hospital experience was too extreme to go into here.
Eventually, I as put on Septra and sent home. It took a few weeks and all seemed well. Another drug was eventually prescribed, called Suprax. This was meant to be a safer alternative. I adjusted to what I considered my "new normal". Within the year, while away from home again, the symptoms came back but I knew how to control them better.
I went to a urologist who confirmed that the E.coli was back. We started the Suprax again. He didn't feel that the two infections were related, even though the E. coli strain was the same. After all the scopes and tests he wanted me to endure, he couldn't find the source. He sent me to an Infectious Disease specialist. This medical Triage team sent me for a battery of more tests and used a lot of my time. I went through an amazing amount of antibiotics. I was on Suprax for 3 years.
The final round of drugs was Ertapenem. The Doctor referred to it as "the bazooka of all antibiotics". Other doctors referred to it as "Javex, Draino and Bleach". I was thinking this would solve it. It was administered for 28 days through an IV drip once a day. 17 days later, all my symptoms were back and raging in a full on attack. I started my stash of Suprax immediately and got the infection under control. The infection specialist was stumped!
While on Suprax there weren't any issues with the infection - but I was taking antibiotics daily with no end in sight. If I stopped and did nothing, the infection would eventually kill me.
The team of doctors recommended a path of surgeries to remove infected parts and tissue to see if they could cut out where the infection was nested. That seemed rather extreme to me. You referred to it as "barbaric." It would only lead to a reduced state of living and a dependency on the medical industry.
Looking for another way through this, my wife found your site and I immediately began reading. Then, I ordered your Uribiotic. I also called you and you advised me. You guided me through the whole process. I used a larger than prescribed amount of supplements as directed by you. You also explained the diet I needed and what other supplements to use.
I stayed the course and did not waiver for 3 months. I called you many times to understand what was happening with me and, as time went by, you adjusted the prescription as needed. It was the first 3 months in years that I didn't take a pharmaceutical antibiotic!
After these 3 months, I couldn't believe that it was over, the infection was gone and not returning.
I waited a few months before writing this note of endorsement. I am amazed and thankful. I have changed my eating habits and added certain supplements to my way of life. I'm not as strict about the diet anymore but I am very strict about the amount of sugar that I will allow myself. My eating habits are much better now. I think I will be amazed for years to come. I never thought I would get through this.
When the specialists suggested the surgery route I said "No." I was going to use your method. They were very skeptical. I told the team of doctors about my recovery and they were astonished. One doctor, who has been practicing his specialty with infections for 27 years, said that I taught him something new!
I thank you. You are a treasure, Mr. Mierzejewski.
Sincerely,
Gordon B.
Toronto, Canada
|
|
Let me start off by saying (and please keep in mind that I rarely submit feedbacks) that I had to send in this positive opinion on Uribiotic Formula and UT ProbioticsUltra. These two paired up equal excellence!
Where do I begin. After having a UTI on and off for way too long that I was never able to cure naturally (stayed away from antibiotics), didn't know what to do next. The infection travelled by body from head to toe. I'm talking strep sore throat almost every month before my monthly cycle, on and off burning sensation when urinating, occasional fevers and chills. On top of that indigestion issues such as belching, gas, low stomach acid, you name it. I could not live like this any longer.
I decided to search the web from top to bottom. Fell on the Uribiotic website and was intrigued by the product right away. I'm willing to invest, I thought. My health has been bad for too long, I said to myself.
Ladies and Gentlemen, Uribiotic and UT ProbioticsUltra have healed me from head to toe!
It has been only one week, but after a few days, my urine is clearer and the burning sensation has decreased by a lot. My strep throat/sore throat is totally gone. Indigestion issues have improved significantly.
Ladies, even my monthly cycle is a breeze!! No cramps!! I am sold and sad that I did not order more bottles. What was I thinking?!
All I can say is: give it a try!!
Melissa D.
Ottawa, Canada
|
|
Dear Uribiotic Team,
I have had recurrent UTI's for the past few years and my doctor usually just gives me Bactrim, which clears it up within 3 days. While on vacation recently I got another one the first day of my trip and panicked because the pain always seems unbearable.
I was able to get another prescription for Bactrim, but after 2 doses (6 days) I felt even worse. Two weeks later and 2 courses of Cipro later I was at my wits end!
My doctor told me there weren't any bacteria in my urine so it could be something else like urethritis or interstitial cystitis. I didn't care what it was, I just wanted to get rid of it and prevent it from ever coming back.
In desperation I went online and researched as much as I could. I found your website and it has been a life-saver.
I started feeling better after the first couple days of taking the Uribiotic Formula, and after the second bottle I was back to normal.
I couldn't believe how fast it worked, and that there were no side effects, like with antibiotics.
Since then I've also started taking your D-Mannose and Probiotic formulas for prevention and I haven't had any UTI symptoms since.
Thank you so much for your very informative website and very effective natural products.
Annie S.
Juneau, AK
|
|
For years I have been plagued with UTI's. Each time trying to fight it off with baking soda, Alka-Seltzer, drinking lots of water and searching the web for natural remedies, only to end up at the dreaded Urgent Care to get antibiotics. Some of them even gave me bad side effects.
I found Uribiotic Formula on my last web search and I read some of the testimonials and thought I would give it a try.
I was amazed! It really, really worked. I didn't go on antibiotics and my infection was cured.
Thank you a million times over! What a freedom to be able to have a natural cure and not have to be on antibiotics...
This product really works and I would highly recommend it to anyone who suffers from UTI.
Laurie S.
Wheelersburg, OH
|
|
Hello, again, Full of Health Team!
I just got on to your website to order more URIBIOTIC... I am the "Katie B." from Denver, Colorado! My testimonial has been on your home page for over 2 years now.
I have been living in China for the past year and I just recently got a bladder infection for the first time in over 2 years!
You have no idea how comforting it has been to have the assurance of having your product in my medicine cabinet while living in such a foreign land with foreign doctors and hospitals.
I was quite scared when I got the bladder infection a couple of days ago, because I thought, "what if it just doesn't work this time and I have to go to a hospital in China?!"
But, have no fear… URIBIOTIC worked for me AGAIN!
THANK YOU FOR YOUR AMAZING PRODUCT!!!! I sing your praises every time I have sex -:)
Thank you and have a great weekend!
Katie
|
|
Thanks, Andrew!
I got a severe bladder infection and also discovered I had an enlarged prostate. I was in bad pain when I often had to go to restroom. One night I was going every 30 minutes.
They put me on sulfa antibiotics and also wanted me to take Flowmax which I told them I would not take. I don't like taking antibiotics if I can help it.
They also did a CAT scan. I took the antibiotics for a few days but they did not help that much.
Until I got my order of Uribiotic in. I started taking it and, after a few days, noticed feeling a little better each day.
I started going to the bathroom about twice a night only. Then just once a night and now I never wake to go to the bathroom. My measured urine outflow in the morning became normal and with no pain.
I was also taking DP Extract for my enlarged prostate for about six weeks. I went to a specialist and he checked me and said that my prostate was normal. He said I don't need to come back.
Now everything is back to normal. I still take both Uribiotic and DP Extract.
I am very thankful for your help and advice, Andrew.
Aaron Hiller
Texas
|
|
Problem solved! The infection is GONE! I just thought you might want to know this in case you get any customers notifying you that URIBIOTIC doesn't seem to be working.
I love your product and continue to rave and refer anyone I talk to about UTIs to your
website.
THANK YOU FOR CREATING THIS PRODUCT!!!
Katie B.
Denver, Colorado
|
Safe and Effective in Animals
|
Hello,
I just wanted to say THANKS so much! I got the Uribiotic Formula and started the treatment. And my dog is doing so much better! No more blood in the urine or getting up at night having to go to the bathroom. She is happy and no more pain.
She have had bladder infections for more than 5 months and the vets had her on some very expensive antibiotics, including Baytril [Enrofloxacin]. And since she is 156 lb. you can imagine how much it cost me to have her on them.
But they were not curing her...
And since I started her on your product she is fantastic! Eating normal again and the life had come back to her body. Thanks so much!
I sent the links to the 2 vets that had seen her and recommended your product if they ever get a dog with a bladder infection resistant to all antibiotics.
Once more, thanks again so much!
Kind Regards,
Isilma H.
California
|
Therapeutic and Preventive Intake: Directions

|
URIBIOTIC FORMULA is a different route to contribute not only to your freedom from urinary tract infections, but also to your optimum urinary health. But when, after reading about this self-help method, you go back to your doctor for an opinion, he or she may say sarcastically, "A herbal antibiotic?! Nonsense! Whom are you going to trust? Some guy on the Internet!? I am your doctor. And as a medical professional, I am responsible for your health." In other words, do what I say or you're going to regret it.
No, this is not an unfair exaggeration. Just the reality we are all in. Not being sure, then, of who's actually giving you the correct information, you may face a real dilemma, a serious problem of trust. However, if - despite following your doctor's routine orders - you are not doing well, then, you should look at your situation honestly and ask yourself, "Am I willing to try a different route?"
It's a well-known fact that no one is immune to well-meaning but sometimes misguided advice from their MDs. Yes, they are professionals with medical degrees - but not with herbalist degrees. Unfortunately, as herbology (along with nutrition) has been excised from the medical school curriculum, most physicians have been, and still are, misinformed or even ill-informed about herbs. For a reason, of course.
Having said all that, with possible variations from person to person - depending on the diagnosis, degree of urinary tract infection, age of the sufferer, and other existing or pre-existing health conditions - the suggested intake of URIBIOTIC FORMULA can be described as follows:
I. Acute UTIs:
In case of first signs of discomfort (slight burning sensation when urinating, frequent urination and/or inability to empty bladder completely) you need to take:
-
4 capsules 3 times daily; therefore, for full benefits, 2 bottles of Uribiotic Formula will be needed.
Our ironclad recommendation: A 6-day therapeutic intake (1 bottle) and, then, an additional 6-day prophylactic intake (1 more bottle) to improve and/or restore the urinary tract’s normal pH, boost the natural safeguards - bodily defense systems that protect the urinary tract against pathogenic, infection-causing bacteria, therefore, to prevent recurring UTIs.
In case persistent signs of UTI (painful burning sensation when urinating, frequent urination at night and/or inability to empty bladder completely) you need to take:
-
4 capsules 3 times daily; therefore, for full benefits, 3 bottles of Uribiotic Formula will be needed.
Our ironclad recommendation: A 12-day therapeutic intake (2 bottles) and, then, an additional 6-day prophylactic intake (1 more bottle) to improve and/or restore the urinary tract’s normal pH, boost the natural safeguards - bodily defense systems that protect the urinary tract against pathogenic, infection-causing bacteria, therefore, to prevent recurring UTIs.
PLEASE NOTE: When acute nephritis (kidney infection) is present - accompanied by high fever along with sudden retention of urine (a painful urge to pass urine but the inability to do so) - have your condition assessed immediately by your physician.
II. Chronic/Repeated UTIs:
In case of recurrent, repeated UTIs (all the above symptoms along with the need and dependence on, or a history of frequent antibiotic use) you need to take:
-
4 capsules 3 times daily; therefore, for full benefits, 4 bottles of Uribiotic Formula will be needed.
Our ironclad recommendation: An 18-day therapeutic intake (3 bottles) and, then, an additional 6-day prophylactic intake (1 more bottle) to improve and/or restore the urinary tract’s normal pH, boo the natural safeguards - bodily defense systems that protect the urinary tract against pathogenic, infection-causing bacteria, therefore, to prevent recurring UTIs.
PLEASE NOTE: When acute nephritis (kidney infection) is present - accompanied by high fever along with sudden retention of urine (a painful urge to pass urine but the inability to do so) - have your condition assessed immediately by your physician.
When to Take Uribiotic: Directions
Take the capsules throughout the day (in the morning - beginning after breakfast, then, at noon, and in the afternoon) away from food, that is either 15 minutes before a meal or about one hour following a meal, each time with ½ glass of purified room-temperature water, preferably alkaline. Both the early eaters and late eaters should have their morning dose of Uribiotic one hour after the first meal of the day (more commonly known as breakfast).
Also, do your best and try to sip lots of water throughout the day, always purified, room-temperature. Why alkaline? Because it has a higher pH level than "regular" water, helps to neutralize acid in the bloodstream, boost metabolism and increase the absorption of nutrients.
Not drinking enough water - an essential, vital nutrient - can increase the risk of urinary tract infections. Dark-yellow urine and/or infrequent urination are some of the symptoms of dehydration - a water imbalance disrupting levels of salts and sugars in the blood, which can interfere with the fundamental bodily functions.
Therefore, adults should consume around six to eight (6-8) cups of fluids or beverages each day. Unfortunately, many women still believe that drinking water causes... fluid retention. In fact, the opposite is true. The body retains water only if there is too little water is the cells. The average adult bladder can hold up to two cups, or 500 mL, of urine for two to five hours.
Cautions and Contraindications
Sexual System:
Uribiotic Formula is not recommended to be taken during pregnancy as it can cause contractions of the uterus due to presence of Goldenseal and hydroquinone (via arbutin present in Uva Ursi/berberine).
Pharmaceutical Drugs:
URIBIOTIC FORMULA should be consumed with caution by patients on a high dose of warfarin (blood thinner) due to the presence, although in an insignificant amount, of garlic which may potentiate the anticoagulant effects of warfarin. (Reference: Fugh-Berman, A. Herb-drug interactions. Lancet. 355(9198):134-138, 2000).
Do Not Stop!
Although symptoms-free, please DO NOT stop taking Uribiotic Formula and continue to use it until all bottles are empty.
If you are prone to repeated/chronic urinary tract infections keep an extra bottle of Uribiotic Formula on hand and use it immediately at the first signs of infection for the minimum of 3 consecutive days, taking 4 capsules 3 times daily.
In time, you will notice that the frequency of your urinary tract infections begins to seize, making the further use of Uribiotic Formula - with some possible exceptions - unnecessary and/or occasional only.
Remember: The Results May Vary
Once again, please note that the results may vary from person depending on the type of diagnosis (urine tests and/or symptoms), the type of bacteria, degree of severity of UTI (ranging from minor to serious), type of UTI (cystitis, urethritis, pyelonephritis), history of antibiotic intake (as this can be a cause of repeated UTIs), structural abnormalities, age, sex and other existing health conditions such as diabetes mellitus and/or any immuno-compromised state. Besides, about half of women with symptoms of a UTI actually have irritation of the urethra, vaginitis, candidiasis, interstitial cystitis, or sexually transmitted diseases (STDs). Some of these problems may also accompany or lead to UTIs.
If Your Infection Persists
In order to enhance the therapeutic, protective and preventive (prophylactic) effects of Uribiotic Formula, especially in case of stubborn, severe and complex urinary tract infections, you may consider taking with it other supporting, bacteria-specific supplements, such as:
| |


Secure Online Order
|
United States and Worldwide (USD)
(Except Denmark, Germany, Mexico, Nigeria, Norway, Saudi Arabia, South Africa, Sweden, Turkey, United Arab Emirates.)
|
|
INTERNATIONAL SHIPPING FEE
(If you are outside the United States)
The website software we use makes it difficult to include a variable international shipping fee for different countries. Therefore, if our cost of shipping to your destination country is significantly different from the Shipping Fee at checkout we will contact you by e-mail with a shipping quote for your approval.
We do not charge for any product until it is ready to ship from our Philadelphia, PA warehouse by U.S. Postal Service (USPS).
Our Promise:
You may rest assured that you will NEVER be put on any automatic reorder scheme!
ONLINE CUSTOMER AGREEMENT
Although Uribiotic is an effective complementary remedy for promoting
urinary tract health and healing, it is not a replacement for conventional medical treatment.
I understand that the information provided herein is not a substitute for medical examination and/or diagnosis; and that is recommended that I see a physician for any physical ailment that I might have and for any new exercise activity, dietary supplementation or diet program that I intend to begin.
I understand that Full of Health, Inc. does not have a money-back guarantee policy and shall not be liable for any issues whatsoever that may arise from the use of/or reliance upon any information obtained and/or any products purchased online through the website of the said company.
By placing my order, I have agreed to accept the conditions of sale contained herein.
|
Concerned About the Cost? Remember:
The bitterness of poor results lingers long after the sweetness of low price.
AmeriCommerce®
Secure Online Payment
|
|

Phone Assistance
If you would like to discuss your ordering options, please give us a call:
- 1. 705. 304. 6246 (US/Can) Mon. Wed. Fri. 11:00 am - 3:00 pm EST (Holidays Excluded).
If there is nobody available to take your call, kindly
click here to email us. We will get back to you next business day.
PLEASE NOTE: If the link above does not respond, it means you are a Mozilla's Firefox web browser user, therefore, this Java plugin has been blocked and disabled on your computer.
PLEASE NOTE: If the link above does not respond, it means you are a Mozilla's Firefox web browser user, therefore, this Java plugin has been blocked and disabled on your computer.
Bladder Infection: Spinal Cord Injuries
Neurological conditions like paraplegia, a spinal cord injury, also called spinal cord impairment (SCI), usually result in a neurogenic bladder - an unstable or atonic bladder (with no muscle tone).
People with spinal cord injuries have lost, partial or complete, control over their bladder and sphincter due to the compromised nerve receptors that are responsible for:
- contracting and relaxing the muscles of the bladder and the sphincter, and
- registering feelings of pressure or release.
Due to this condition, most paraplegics are exposed to the regular use of catheters and drugs. (The more traditional cap and bag, with continual drainage, is falling from favor even though it is a safer system).
However, catheters often increase the risk of the urinary tract injuries and repeated bladder infections - a common problem in people with spinal cord impairment.
Exposed to repeated or long-term courses of antibiotics, in time, they also develop resistance to drugs what makes maintaining healthy urinary tract for them even more difficult.
Contrary to a popular belief and common medical practice, people with spinal cord injuries or spinal cord impairment do NOT have to:
- suffer from chronic bladder-kidney infections and
- be exposed to vicious antibiotics.
It is our clinical experience that paraplegics, expecially those who use catheters, can successfully remedy, and most importantly, prevent bladder-kidney infections with the help of our proprietary UTI Uribiotic Formula.
Therefore, you, or someone you know or hold dear, who suffers from spinal cord injury, should give this superb herbal blend serious consideration.
People with SCI Write to Us
I have been quadriplegic for 15 years. About seven years ago, I started to suffer recurrent urinary tract infections to the point where most of the bacteria had become multiresistant.
My urologist pointed out to me that kidney failure is the biggest killer of people with spinal cord injuries as a result of repeated urinary tract infections which became untreatable as a result of repetitive use of antibiotics.
About two years ago I developed an infection, the bacteria being pseudomonas. Antibiotics did not work and the decision was made to not use any more, live with it and hope it didn't get into my bloodstream.
I couldn't accept this, so I researched the Internet once again until I finally found out about oil of oregano and Uribiotic. I ordered some, showed my GP who confirmed that there was nothing in it that could possibly cause any harm and to give it a go, which I did.
Within a few weeks the urinary tract infection cleared up.
I have barely had any symptoms since, and when I do I just use the Uribiotic for a couple of days and symptoms clear up. No side effects and no worries about the tablets not working.
I am a skeptic and honestly didn't think this would work when I tried it, but it does. If I didn't find out about it, I hate to think where I would be now.
I just wish I knew about it sooner.
Janine P.
Western Australia
|
Thanks, Andrew, for your advice and support with my Pseudomonas [aeruginosa] bladder infection with your amazing product Uribiotic which stopped the infection and kept it away.
I've suffered from UTIs for 18 years since my spinal cord injury and now I'm infection free.
JASON C.
Great Britain
|
As a paraplegic for almost 14 years, I was almost constantly on antibiotics due to chronic bladder infection. However, being afraid of possible side effects, for many years I was reluctant to consider any natural alternatives.
I was afraid of getting diarrhea or constipation. These are the worst - a real disaster! But after successful experience with D-Mannose, I started looking for other natural means to solve my problem.
And I was pleasantly surprised by lack of any adverse reactions to URIBIOTIC, which I introduced to my system very cautiously.
Two weeks later, my urine culture showed NO E. coli. Burning went away in a
few days. I'm pleased to report such great results.
Barret D.
Minnesota
|
Advanced Urinary Tract Support: Naturopathic Program
 NEED HELP OR ADVICE?
NEED HELP OR ADVICE?
Contact us by  or by phone: 1. 705. 304. 6246 (US/Can) or by phone: 1. 705. 304. 6246 (US/Can)
Mon. Wed. Fri. 11:00 am-3:00 pm EST (Holidays Excluded)
 © 2003-2021 Remedy-Bladder-Infection.com. Stop Urinary Bladder Infection with UTI Uribiotic Formula. Advanced Urinary Tract Support. Holistic Natural UTI Cure, Treatment & Prevention. Bladder infection herbal treatment for cystitis, urethritis, and urethral syndrome. The information on bladder infection and the natural alternatives to antibiotics provided herein is a general overview on bladder infection and may not apply to everyone; therefore, it should not be used for diagnosis or treatment of any medical condition. While reasonable effort has been made to ensure the accuracy of the information on bladder infection, Full of Health Inc. assumes no responsibility for errors or omissions, or for damages resulting from use of the UTI information herein.
© 2003-2021 Remedy-Bladder-Infection.com. Stop Urinary Bladder Infection with UTI Uribiotic Formula. Advanced Urinary Tract Support. Holistic Natural UTI Cure, Treatment & Prevention. Bladder infection herbal treatment for cystitis, urethritis, and urethral syndrome. The information on bladder infection and the natural alternatives to antibiotics provided herein is a general overview on bladder infection and may not apply to everyone; therefore, it should not be used for diagnosis or treatment of any medical condition. While reasonable effort has been made to ensure the accuracy of the information on bladder infection, Full of Health Inc. assumes no responsibility for errors or omissions, or for damages resulting from use of the UTI information herein.
URIBIOTIC and FULL OF HEALTH are registered trademarks of Full of Health, Inc.
|















 NEED HELP OR ADVICE?
NEED HELP OR ADVICE? or by phone: 1. 705. 304. 6246 (US/Can)
or by phone: 1. 705. 304. 6246 (US/Can) © 2003-2021 Remedy-Bladder-Infection.com. Stop Urinary Bladder Infection with UTI Uribiotic Formula. Advanced Urinary Tract Support. Holistic Natural UTI Cure, Treatment & Prevention. Bladder infection herbal treatment for cystitis, urethritis, and urethral syndrome. The information on bladder infection and the natural alternatives to antibiotics provided herein is a general overview on bladder infection and may not apply to everyone; therefore, it should not be used for diagnosis or treatment of any medical condition. While reasonable effort has been made to ensure the accuracy of the information on bladder infection, Full of Health Inc. assumes no responsibility for errors or omissions, or for damages resulting from use of the UTI information herein.
© 2003-2021 Remedy-Bladder-Infection.com. Stop Urinary Bladder Infection with UTI Uribiotic Formula. Advanced Urinary Tract Support. Holistic Natural UTI Cure, Treatment & Prevention. Bladder infection herbal treatment for cystitis, urethritis, and urethral syndrome. The information on bladder infection and the natural alternatives to antibiotics provided herein is a general overview on bladder infection and may not apply to everyone; therefore, it should not be used for diagnosis or treatment of any medical condition. While reasonable effort has been made to ensure the accuracy of the information on bladder infection, Full of Health Inc. assumes no responsibility for errors or omissions, or for damages resulting from use of the UTI information herein.


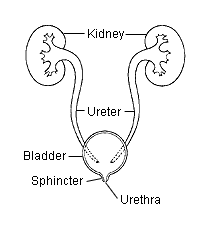

 Since 2004, we have been supplying with our proprietary Uribiotic Formula clients and customers in 34 countries: the United States, Australia, the United Kingdom, South Africa, New Zealand, Germany, Belgium, Mexico, Italy, Singapore, France, Russia, Croatia, Poland, Portugal, Denmark, United Arab Emirates, Hong Kong, St. Lucia (West Indies), Norway, Saudi Arabia, Turkey, Slovenia, Greece, Qatar, Jordan, Israel, the Netherlands, Luxembourg, Sri Lanka, India, Spain, China, and Chile.
Since 2004, we have been supplying with our proprietary Uribiotic Formula clients and customers in 34 countries: the United States, Australia, the United Kingdom, South Africa, New Zealand, Germany, Belgium, Mexico, Italy, Singapore, France, Russia, Croatia, Poland, Portugal, Denmark, United Arab Emirates, Hong Kong, St. Lucia (West Indies), Norway, Saudi Arabia, Turkey, Slovenia, Greece, Qatar, Jordan, Israel, the Netherlands, Luxembourg, Sri Lanka, India, Spain, China, and Chile.

